Beyond the AI Hype: Building Trust at Scale
Combining Human Connection with AI Capabilities to Transform Chronic Care
Despite the AI hype in healthcare, technology alone won't solve our most fundamental challenges. The most promising path forward isn't replacing human expertise with AI—it's something more nuanced and powerful.
Our healthcare system has a chronic care problem: excellent at acute interventions but missing critical opportunities between clinical visits. What if we could combine the irreplaceable elements of human care with the scalability of technology?
The future of healthcare isn't an either/or proposition. The real breakthrough comes from thoughtful integration that preserves trust while expanding access and personalization.
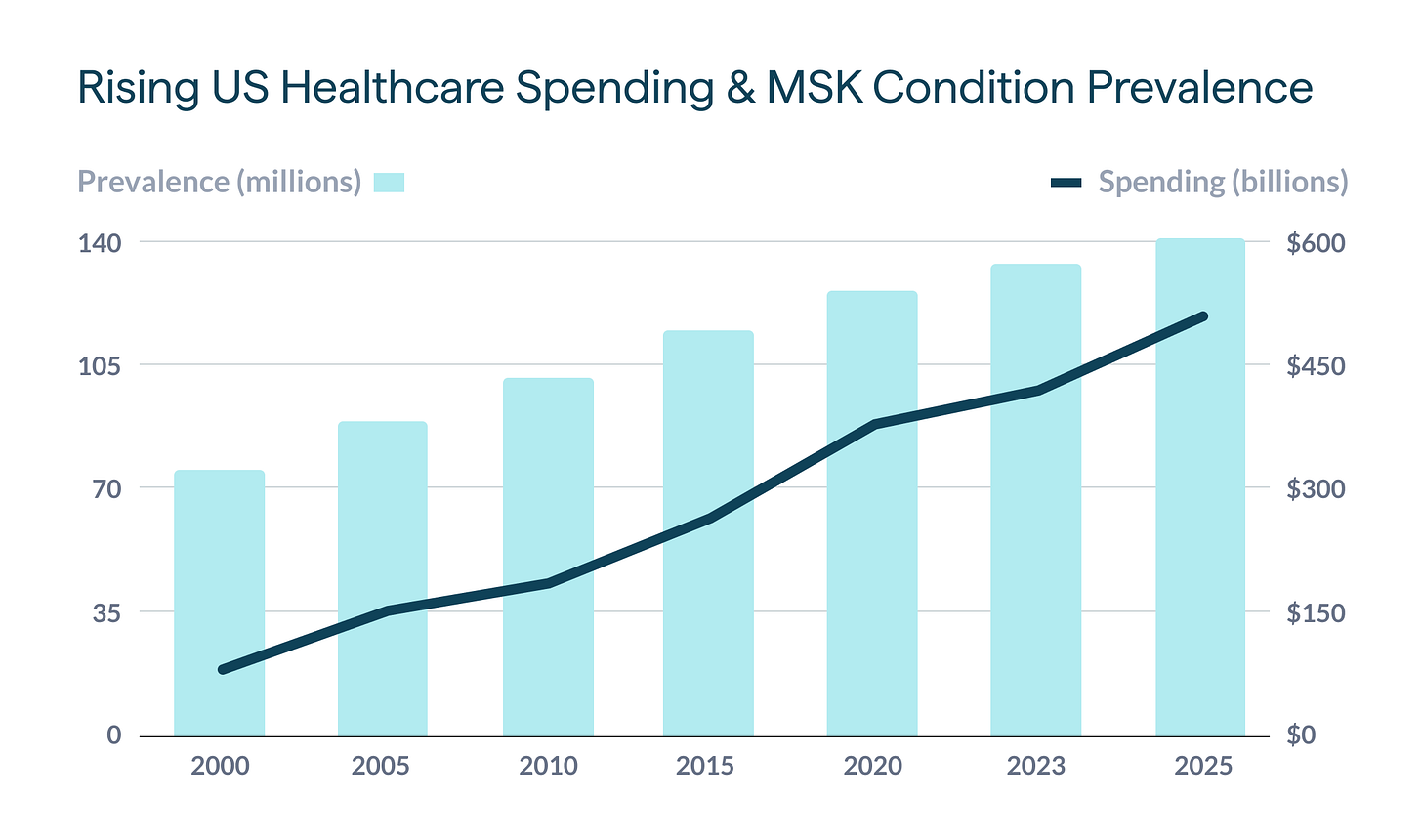
We're witnessing a fundamental challenge in healthcare today: despite skyrocketing spending1 and technological advances, millions of Americans with chronic physical conditions still lack the ongoing support they need between clinical visits. Our healthcare system excels at acute interventions but falls short when it comes to the continuous, personalized care that chronic conditions demand.
This disconnect is particularly pronounced for people with musculoskeletal conditions. Whether it's osteoporosis, arthritis, or chronic back pain, these conditions require consistent, evidence-based interventions that our episodic care model simply doesn't provide.
The Triple Challenge: Why Healthcare Needs Reimagining
Today's healthcare system faces three intersecting challenges that create critical care gaps:
First, our system remains deeply fragmented. We've moved further from centralized, whole-person care as our system has evolved into a splintered network of specialized practices with convoluted reimbursement codes.2 This fragmentation creates significant gaps in care continuity, particularly between clinical visits when people need ongoing support.
Second, there's a widening disconnect between clinical recommendations and real-world implementation. When a provider recommends "exercise more" or "strengthen your core," patients typically receive little guidance on how to execute these instructions safely and effectively. This lack of specificity and support leads to poor adherence and suboptimal outcomes.
Third, our current approach to behavior change often relies on information alone, ignoring the critical role of accountability, motivation, and personalization. Knowledge about what to do rarely translates into consistent action without the right support system in place.
AI Alone Isn't the Answer
With the explosion of artificial intelligence, many have positioned AI as healthcare's savior—promising personalization at scale, 24/7 accessibility, and dramatic cost reductions. The hype cycle suggests we'll soon have AI doctors in our pockets, eliminating the need for human providers entirely.
But this techno-optimism misses something fundamental: health is deeply personal and intimate. People's health journeys are complex, filled with nuances that even the most sophisticated algorithms struggle to comprehend. Trust remains foundational to effective healthcare relationships, and accountability that feels human and personal drives behavioral change in ways that automated reminders simply cannot replicate.
The question isn't whether AI can replace human healthcare providers—it's how we can combine human expertise with AI capabilities to create something better than either could achieve alone.
"The greatest opportunity offered by AI is not reducing errors or workloads, or even curing cancer: it is the opportunity to restore the precious and time-honored connection and trust." - Dr. Eric Topol
The Middle Path: Human-AI Partnership in Condition-Specific Care
At Groove Health, we're pioneering a different approach—one that leverages both human expertise and AI capabilities to deliver condition-specific care that's both high-touch and scalable.
Our model recognizes that physical health challenges aren't monolithic. Instead, we provide targeted, evidence-based exercise programs designed specifically for each person's condition, goals, and life circumstances. Rather than offering generic wellness advice, we focus on specific musculoskeletal conditions where tailored interventions can make transformative differences.
This condition-specific approach allows for several critical advantages:
Precise calibration of interventions: Exercises and protocols tailored to the exact physiological needs of specific conditions
Relevant education and guidance: Information contextualized to the person's unique health situation
Appropriate risk management: Careful consideration of contraindications and safety concerns specific to each condition
Meaningful progress metrics: Tracking improvements in ways that matter for the particular condition
The power of this approach comes from combining human coaching relationships with AI-enhanced personalization. Our human coaches build trust, provide accountability, and offer the empathy and understanding that only humans can provide. Meanwhile, our technology layer helps personalize plans, track progress, and scale our coaches' expertise to make care more accessible and affordable.
Case Study: Revolutionizing Osteoporosis Care
Our recently launched osteoporosis and osteopenia solution demonstrates this approach in action. Bone health represents an area where conventional care often falls short—typically limited to medication prescriptions and vague advice to "do weight-bearing exercise" without specific guidance.
Yet the potential impact of proper intervention is enormous. Research shows that regular exercise can reduce fracture risk by 51%.3 Our program combines expert-designed workouts specifically for bone health, personal coaching that builds and adapts each plan, and targeted education about nutrition and strength.
The results speak for themselves: 95% of our users report increased strength and confidence within just six weeks. This isn't just subjective improvement—it translates to measurable reductions in fall risk and improved functional capacity for daily activities.4
What makes this possible is our human-in-the-loop model. Each member receives regular video check-ins with their coach, who reviews their form, provides immediate feedback, and ensures proper technique. This human relationship creates the trust and accountability necessary for consistent engagement, while our technology platform makes personalization scalable and the service affordable.
The Future: Scaling Trust and Expertise
As we look to the future of healthcare for chronic physical conditions, we're confident that the most effective solutions will take this middle path—combining human expertise with technological capabilities to create care models that are both high-touch and scalable.
The engagement metrics we're seeing validate this approach. On average, 92% of our users engage every day, 85% complete their individualized weekly plan, and over 80% continue with the program for six months or more. These numbers far exceed typical digital health engagement rates and speak to the power of human-technology partnerships.
In the coming months, we'll be expanding our condition-specific offerings to address additional musculoskeletal challenges, including back pain—another area where conventional care often leaves significant gaps.
Bridging the Gaps in Care
The future of healthcare isn't about choosing between human providers or AI tools—it's about creating thoughtful combinations that leverage the strengths of each to bridge the gaps in our current system.
In a healthcare landscape increasingly defined by fragmentation, rising costs, and diminishing personal connections, we need solutions that rebuild trust, provide continuous support, and deliver measurable outcomes. By creating services that are rooted in science, powered by tech, and delivered by people who care, we can transform how people experience healthcare.
The AI revolution in healthcare isn't about replacing humans—it's about enhancing human connections and making expert relationships more accessible to everyone who needs them. That's the future we're building at Groove Health, one condition-specific solution at a time.
What do you think? I'm curious to hear your perspective on the role of human-AI partnerships in healthcare. Have you experienced gaps in care for chronic conditions? What solutions have you found most effective?
Share your thoughts in the comments, or reach out directly if you'd like to discuss how we're approaching these challenges at Groove Health.
Patrick Weiss is the co-founder and CEO of Groove Health, a digital health company pioneering human-AI partnerships for condition-specific care. Groove combines expert coaching with technology to provide continuous, personalized support for people with chronic musculoskeletal conditions, helping them reduce pain and improve strength, mobility, and balance. Learn more at groovehealth.com.
Chart: Prevalence of Musculoskeletal Conditions and Associated Healthcare Spending in the United States, 2000-2025. Data compiled from multiple sources: United States Bone and Joint Initiative (2016, 2020); Cleveland Clinic Global Burden of Disease Analysis (2022); Evernorth MSK Total Cost of Care Report (2023). 2025 and years without published data points represent interpolated estimates based on reported growth trends.
Hyman, D. A., & Silver, C. (2021). Healthcare fragmentation: A cross-national analysis of the consequences for patient care. Health Policy, 125(5), 567-579. doi:10.1016/j.healthpol.2020.11.008
Zhao, R., Feng, F., & Wang, X. (2017). Exercise interventions and prevention of fall-related fractures in older people: a meta-analysis of randomized controlled trials. International Journal of Epidemiology, 46(1), 149-161. doi:10.1093/ije/dyw142
Daly RM, Dalla Via J, Duckham RL, Fraser SF, Helge EW. Exercise for the prevention of osteoporosis in postmenopausal women: an evidence-based guide to the optimal prescription. Braz J Phys Ther. 2019 Mar-Apr;23(2):170-180. doi: 10.1016/j.bjpt.2018.11.011. Epub 2018 Nov 22. PMID: 30503353; PMCID: PMC6429007.


